I Won’t Stop Talking about My Uterus
From a high-risk pregnancy at 32 to menopause at 48, Aileen Weintraub has learned she mustn't shut up about her reproductive health until the medical establishment prioritizes women.
“So, what was it like being on bed rest for five months?” asked the journalist. She was interviewing me over Zoom about my new book Knocked Down: A High-Risk Memoir. I could feel beads of sweat forming on my forehead. My skin was burning and I had to quell the desperate desire to rip off my clothes and run outside into the cold winter air. I was having my third hot flash of the day, and I knew more would follow in rapid succession.
I paused for a moment as if considering the question, secretly wondering how I, at age 48, could sit here discussing my high-risk pregnancy, which occurred 16 years ago, while I’m now smack in the middle of menopause.
As I settled into the interview, I began explaining the difficulties of being on bed rest. Inwardly, I was making undeniable parallels between that time of my life and my current experience as a middle-aged woman. I didn’t feel seen or heard by the healthcare community back then, and I certainly didn’t now, as my body continued to betray me.
I paused for a moment as if considering the question, secretly wondering how I, at age 48, could sit here discussing my high-risk pregnancy, which occurred 16 years ago, while I’m now smack in the middle of menopause.
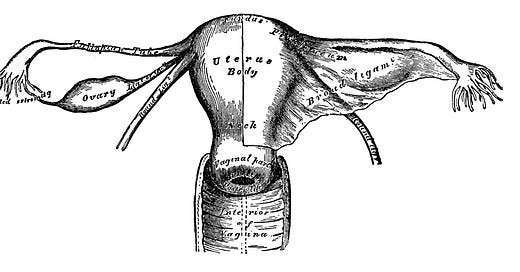
It occurred to me while I was speaking that I’ve always liked to talk about my uterus. That fascination began when I was 32. I was four months pregnant walking around New York City with my new husband when I felt a sharp pain in my lower belly. I called my OBGYN, and a nurse dismissed my concerns telling me to wait until the following day for my already scheduled visit. Once my OBGYN examined me, things moved quickly and I was rushed off to an emergency sonogram. I had three monster-sized fibroids growing in my uterus right alongside the baby, and one of them was pressing on my cervix causing early effacement. The doctor told me that I’d be lucky if my baby made it to twenty-four weeks. The next five months in bed was a lifechanging experience that stripped me of my autonomy, my career, and my financial stability. It wasn’t great for my young marriage either.
When my son, who was born healthy and on his due date, turned five, I knew I had to address the trauma that bed rest had caused. So I wrote Knocked Down.
During those years of writing about my uterus and all the problems that went along with it, I also began to focus on broader issues women face, whether as a children’s book author writing about the lack of equality in women’s sports, or as an essayist revealing the loneliness and feelings of invisibility during both perimenopause and menopause. Now, I was discovering that these issues all had one thing in common: there is simply not enough awareness around them. While doing the Zoom interview I realized that no matter what I am writing about, my goal remains the same. I want women to feel seen and heard.
A New York Times article suggests that menopause is studied for one single hour in medical school. This life-changing event, which affects almost every single woman in the entire world, gets only sixty minutes of attention.
My doctor didn’t warn me about the mental and physical effects five months in bed would have on my mind or my body. Nor did anyone prepare me for the roller coaster ride perimenopause would bring. I didn’t even know what perimenopause was until I called my doctor and told her I thought I was dying because I couldn’t remember words, had left boob pain, and rage that made me feel like I was a walking volcano ready to spew lava.

A New York Times article suggests that menopause is studied for one single hour in medical school. This life-changing event, which affects almost every single woman in the entire world, gets only sixty minutes of attention. Want to talk about rage now? It’s not just menopause, though. As I mentioned to my Zoom interviewer, years before, when my doctor dropped the news that I would have to spend five months in bed if I wanted to save the life of my unborn baby, I tried googling studies about bed rest. Those studies were sorely lacking, and sixteen years later they still are. At the time, I actually googled “stupid scientific studies” to see where we were spending our money instead. You don’t even want to know.
When I speak to other women about their health care experiences, they consistently tell me that their doctors dismiss their concerns or blame their symptoms on anxiety. Maybe we wouldn’t have so much anxiety if more people listened to us. Maybe it’s not anxiety at all, but gaslighting, which studies show is common when it comes to women’s health. After my child was born, I experienced a terrible pounding in my ears, I couldn’t sleep, and there were days I only got out of bed because I was the caregiver and I had no other choice. Predictably, my general practitioner shrugged it off when I mentioned it. It wasn’t until years later that I finally figured out on my own that I had been suffering from postpartum depression.
When I speak to other women about their health care experiences, they consistently tell me that their doctors dismiss their concerns or blame their symptoms on anxiety.
I had a similar experience recently at an annual visit to my OBGYN when I mentioned what I finally understood to be symptoms of menopause. I had memory loss, sleeplessness, and never-ending hot flashes. She told me that if I wanted to discuss it, I would have to come back for another appointment. I said to her, “This is the appointment. This is why I’m here.” She only replied that it wasn’t included in my annual visit. I never went back.
The medical community has a long way to go in getting up to speed with women’s health concerns. So how do we fix this? I don’t pretend to know the answer, but I can say this: We keep telling our stories. We demand to be heard. We don’t take no for an answer, and we support and validate other women’s lived experiences...loudly. It is only by giving light and space to our trauma, by letting it breathe, by continuing to advocate, and by talking to one another that we can facilitate real change. That’s why I’m never going to stop talking about my uterus.






I hear you, and feel more heard by you writing about your experiences. Thank you.
I recommend Heather Corinna’s book on perimenopause and menopause unreservedly! https://www.hachettego.com/titles/heather-corinna/what-fresh-hell-is-this/9780306874758/